


Is Your Pregnancy at Risk? Uncover the Hidden Dangers of Gestational Diabetes!
Gestational diabetes is an important health concern affecting approximately 2-10% of pregnant women. It is usually seen during the second or third trimester and can pose serious risks to both mother and baby if not treated immediately. The aim of this article is to educate expectant mothers on the causes, symptoms, management strategies, and potential complications of gestational diabetes, empowering them to take control of their health during pregnancy.
What is Gestational Diabetes?
Gestational diabetes is a kind of diabetes that occurs during pregnancy when the body cannot produce enough insulin to meet the increased demands of pregnancy. Insulin is a hormone produced by the pancreas that helps regulate blood sugar levels. When insulin levels are insufficient, blood sugar levels rise, leading to hyperglycemia. This condition can have serious implications for both the mother and her baby.
Causes and Risk Factors of Gestational diabetes
● Hormonal Changes: During pregnancy, hormone shifts can mess with how your body uses insulin, making it harder for it to do its job properly.
● Weight Gain: If you’re already overweight before pregnancy or end up gaining a lot while pregnant, it can increase the risk of issues with insulin.
● Family History: Having a family history of diabetes, especially type 2, can raise the chances of developing gestational diabetes.
● Age: Women over 25 have a higher risk of developing gestational diabetes.
● Previous history: If you had gestational diabetes in a past pregnancy, you’re more likely to experience it again.
Recognizing Symptoms
● Increased thirst
● Frequent urination
● Fatigue
● Nausea or vomiting
● Blurred vision
If you notice any of these symptoms, be sure to check in with your healthcare provider for a thorough evaluation and testing.
Diagnosis of Gestational Diabetes
Gestational diabetes is usually identified with a glucose screening test conducted between the 24th and 28th weeks of pregnancy. The test starts with drinking a sweet glucose solution, followed by a blood test to check your blood sugar levels. If the results show higher levels than normal, your doctor might recommend a follow-up test called an oral glucose tolerance test (OGTT) to confirm the diagnosis.
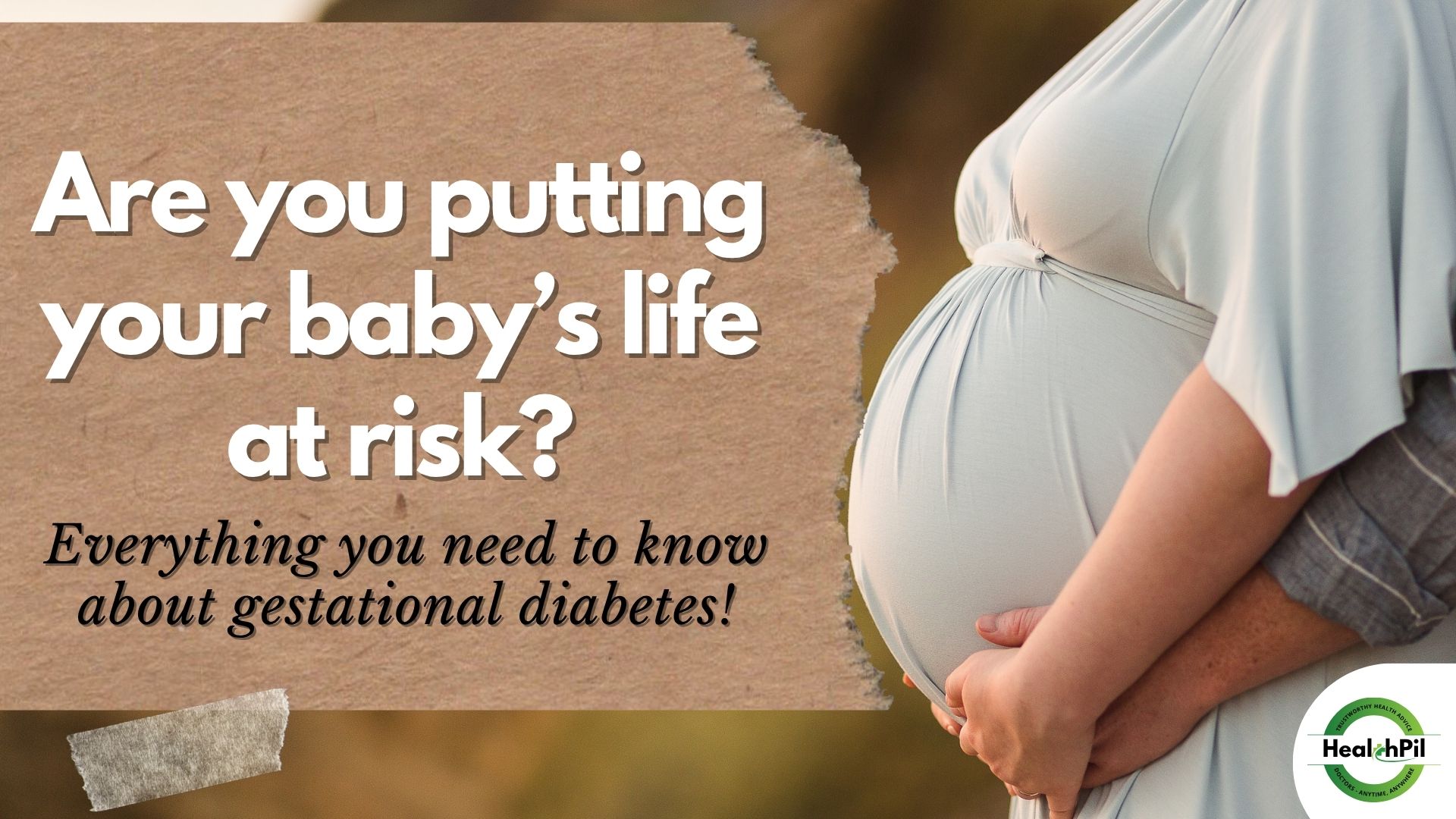
Potential Risks and Complications
If left unmanaged, gestational diabetes can lead to several complications for both mother and baby, including:
● Macrosomia: When a mom has gestational diabetes, her baby may face some extra health challenges after birth such as growing larger than average (a condition called macrosomia), which can complicate delivery and increase the likelihood of cesarean sections.
● Preterm Birth: Elevated blood sugar levels can lead to preterm labor and delivery.
● Low Blood Sugar (Hypoglycemia): After birth, babies may experience low blood sugar levels if their mothers had gestational diabetes.
● Increased Risk of Type 2 Diabetes: Having had gestational diabetes increases a woman’s chances of developing type 2 diabetes in future.
Management and Treatment
1. Dietary Modifications:
● Balanced Meals: Rely on a diet full of whole grains, lean proteins, fruits, and veggies, and steer clear of processed sugars.
● Portion Control: Try eating smaller, more frequent meals throughout the day to help keep your blood sugar levels in check.
2. Regular Monitoring:
● Blood Sugar Monitoring: Regularly monitor your blood sugar levels as recommended by your healthcare provider. This can help you understand how your body responds to different foods and activities.
● Record Keeping: Maintain a log of your blood sugar readings, dietary intake, and physical activity to share with your healthcare team.
3. Physical Activity:
● Exercise:
● Try to include regular activities like walking, swimming, or even prenatal yoga. Aim to get at least 30 minutes of moderate exercise on most days, but always check with your doctor to make sure it’s safe for you.
4. Medical Intervention:
● Insulin Therapy: If dietary changes and exercise are insufficient to manage blood sugar levels, your healthcare provider may prescribe insulin injections to help regulate your blood sugar.
Importance of Regular Check-ups
Regular antenatal check-ups are crucial for monitoring the health of both mother and baby. During these appointments, your doctor will monitor your blood sugar levels, weight, and overall health. They’ll also offer tips for managing gestational diabetes and make sure to address any questions or concerns you might have.
Frequently Asked Questions
What causes gestational diabetes?
Gestational diabetes occurs due to hormonal changes during pregnancy that affect insulin function. It can also be influenced by factors such as obesity and family history.
How is gestational diabetes diagnosed?
A glucose screening test is typically performed between 24-28 weeks of pregnancy. If necessary, a follow-up oral glucose tolerance test (OGTT) will confirm the diagnosis.
What are the risks of untreated gestational diabetes?
Untreated gestational diabetes can lead to complications such as macrosomia, preterm birth, and increased risk of type 2 diabetes for the mother.
How can I manage gestational diabetes?
Management includes dietary modifications, regular blood sugar monitoring, physical activity, and, in some cases, insulin therapy.
Can gestational diabetes go away after delivery?
Yes, gestational diabetes usually resolves after delivery, but women who have had it are at increased risk of developing type 2 diabetes later in life.
Conclusion
Gestational diabetes is a serious condition that requires attention and management. By understanding the risks, recognizing the symptoms, and adopting a proactive approach, expectant mothers can ensure a healthier pregnancy for themselves and their babies. Regular check-ups and open communication with healthcare providers are essential in navigating this journey.
Disclaimer
The information provided in this article is for awareness purposes only and should not replace professional medical advice. Always consult your healthcare provider for personalized medical guidance.
How HealthPil can help?
HealthPil Is Always Here for YOU!
● Need Guidance? Connect with healthcare experts ready to help you navigate gestational diabetes.
● Join Our Community: Gain access to tips, resources, and support from mothers just like you!
● Don’t Delay—Take Action! Your health and your baby’s future are too important to wait!
Contact HealthPil today and empower your pregnancy journey!