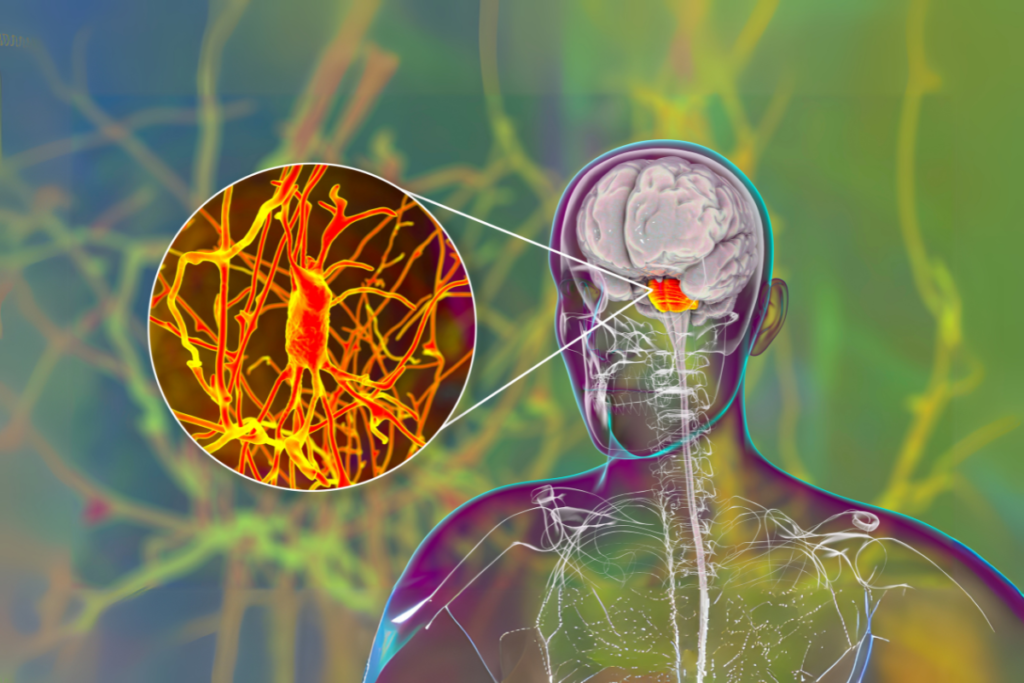
Imagine waking up one day, feeling like you’re losing control over your own mind—struggling to remember things, speaking gibberish, or experiencing sudden mood changes. It could be autoimmune encephalitis, a rare but probably deadly brain condition that can worsen quickly.
What is autoimmune encephalitis?
A dangerous neurological disorder known as autoimmune encephalitis occurs when the body’s immune system unintentionally attacks the brain. The brain’s regular processes may be disrupted, and inflammation may result from this attack, which could cause sudden and drastic changes in memory, thinking, and behaviour.
The condition is relatively rare but extremely dangerous if not recognised and treated promptly. As a neurologist, I’ve witnessed the rapid progression of autoimmune encephalitis, where patients can go from normal function to being unable to speak, move, or recognise loved ones in a matter of days.
Symptoms of Autoimmune Encephalitis: What to Look For
The symptoms of autoimmune encephalitis can vary greatly depending on the part of the brain affected, but common signs include:
● Cognitive Dysfunction: Memory loss, confusion, and difficulty thinking clearly or following conversations.
● Psychiatric Symptoms: Unexplained mood swings, anxiety, paranoia, and even psychosis (e.g., hallucinations or delusions).
● Seizures: Sudden onset of seizures, which can occur without warning.
● Movement Problems: Difficulty speaking, involuntary movements, or abnormal gait (walking).
● Fluctuating Consciousness: A person may have difficulty staying awake, be unusually drowsy, or exhibit periods of confusion.
● Autonomic Dysfunction: Symptoms like irregular heart rate, low blood pressure, or breathing problems can occur in severe cases.
These symptoms may develop gradually, or they can appear suddenly. Because the symptoms can resemble psychiatric disorders or other neurological conditions, the diagnosis is often delayed, which is why early recognition is critical to avoid permanent damage.
How Is Autoimmune Encephalitis Diagnosed?
Neurologists diagnose probable cases of autoimmune encephalitis using a variety of methods.
1. Medical History and Clinical Examination:
The first step is to review the patient’s symptoms and medical history. We look for signs such as:
● Recent infections (e.g., viral illnesses that may trigger an immune response).
● New-onset psychiatric symptoms or unexplained cognitive decline.
2. Blood Tests and Antibody Screening:
The detection of autoantibodies in the blood that target certain brain receptors is an important diagnostic step in blood tests and antibody screening. The following antibodies are commonly linked to autoimmune encephalitis:
● Anti-NMDA receptor antibodies: Often associated with anti-NMDA receptor encephalitis, which is a common form of autoimmune encephalitis.
● Anti-LGI1 and Anti-CASPR2 antibodies: Linked to other types of autoimmune encephalitis.
These antibodies are often the first clue pointing to an autoimmune cause, as they are not typically found in other conditions.
3. Lumbar Puncture (Spinal Tap):
A lumbar puncture to collect cerebrospinal fluid (CSF) is done to assess for inflammation and immune activation in the brain. In autoimmune encephalitis, the CSF typically shows:
● Elevated white blood cells (a sign of inflammation).
● Elevated protein levels.
● Normal glucose (distinguishing it from infections like meningitis).
4. Neuroimaging (MRI/CT Scan):
Any abnormalities in the brain caused by inflammation can be found with the help of an MRI scan. But, since MRI results in autoimmune encephalitis can often be normal, they are mostly used to rule out other possible causes, such as stroke or malignancies.
5. Electroencephalogram (EEG):
EEG can be useful for detecting seizure activity, which is common in autoimmune encephalitis. It can help distinguish autoimmune encephalitis from other causes of seizures or altered mental status.
Treatment: How to Fight Back Against Autoimmune Encephalitis
Early intervention is important in treating autoimmune encephalitis. If you don’t get it treated, it can lead to permanent brain damage, severe cognitive deficits, or even death. The main goals of treatment are to help the patient’s recovery while controlling the immune system’s attack on the brain.
1. Immunotherapy:
The cornerstone of treatment for autoimmune encephalitis is immunotherapy, which aims to suppress the immune system’s abnormal response.
● High-dose corticosteroids (e.g., methylprednisolone) are often the first-line treatment to reduce inflammation.
● Plasmapheresis (plasma exchange) is used to remove harmful antibodies from the blood, especially in severe cases.
● Intravenous immunoglobulin (IVIg) therapy is another option, providing healthy antibodies to regulate the immune system.
2. Seizure Control:
If the patient is having seizures, antiepileptic medications (e.g., levetiracetam or valproic acid) are used to control them and prevent further brain damage.
3. Supportive Care:
In addition to specific treatments for the immune system, supportive care is essential:
● Antipsychotic medications may be prescribed for severe psychiatric symptoms like agitation or delusions.
● Cognitive and physical therapy help patients recover cognitive functions and regain mobility.
4. Treatment for Underlying Triggers:
If an infection or cancer is suspected to be triggering the autoimmune response, that condition must be treated as well.
Prognosis: Can Autoimmune Encephalitis Be Reversed?
With early treatment, many patients experience significant recovery. However, the severity of the brain damage and the quickness at which treatment is started decide how much recovery is possible.
● Mild to moderate cases: Many patients recover well, though it can take months of treatment and therapy.
● Severe cases: Some patients may experience long-term cognitive and psychiatric symptoms, even after the infection has been treated.
How to Care for a Patient with Autoimmune Encephalitis
Caring for a loved one with autoimmune encephalitis can be overwhelming, especially since the symptoms can fluctuate and cause significant distress. Here’s how to help:
1. Monitor Symptoms:
Watch for changes in behaviour, memory, and alertness. Any worsening of confusion, seizures, or physical function should be reported to a healthcare provider immediately.
2. Support Mental Health:
Patients may feel confused or have mood changes. Support them emotionally and with encouragement as they heal.
3. Encourage Rehabilitation:
Cognitive therapy and physical rehabilitation are essential to recovery. Encourage the patient so that they participate in therapy to help regain their strength and cognitive abilities.
4. Medication Adherence:
Ensure that the patient takes all prescribed medications regularly to manage inflammation, seizures, and psychiatric symptoms.
How HealthPil Can Help:
At HealthPil, we understand how frightening autoimmune encephalitis can be. FOurneurologists specialise in early diagnosis and tailored treatment. For autoimmune encephalitis We give teleconsultations to deliver professional care when it’s convenient for you, whether you’re dealing with a possible case or need advice on continued management.
We can help you or your loved ones overcome this difficult condition and seek recovery with prompt action and complete treatment.
FAQ
How quickly can autoimmune encephalitis progress?
It may take days or weeks for symptoms to appear. It can sometimes worsen quickly, resulting in seizures, neuropsychiatric symptoms, and severe memory loss.
Is autoimmune encephalitis treatable?
Many people recover if they are diagnosed early and receive appropriate immunotherapy. However, to avoid permanent harm, quick action is important.
Can autoimmune encephalitis be fatal?
Without prompt treatment, autoimmune encephalitis can be life-threatening. However, with appropriate treatment, the mortality rate has decreased greatly.
Are there any long-term effects after recovery?
While many patients recover fully, some may experience lingering cognitive issues, memory problems, or psychological symptoms that require ongoing care.
Can autoimmune encephalitis happen again?
It can recur, particularly if the underlying cause (e.g., an infection or malignancy) is not addressed. Regular follow-up care is important to monitor for relapse.
Disclaimer:
This article is for informational purposes only and should not be considered medical advice. Always seek immediate medical attention if you suspect autoimmune encephalitis or any other neurological condition.